How Healthcare Firms Optimize AR

Healthcare organizations struggle with delayed payments, impacting cash flow and financial health. Accounts Receivable (AR) management is critical to maintaining stability. Here's a quick breakdown of how top-performing providers tackle AR challenges:
- Target Days Sales Outstanding (DSO): Aim for 30–40 days. Reducing DSO from 50 to 40 days can release millions in liquidity for large hospitals.
- Key Challenges: High claim denial rates (12–18%), low patient collection rates (around 48%), and over 20% of AR unpaid after 90 days.
- Solutions:
- Clear Payment Policies: Require upfront payments for co-pays and deductibles. Use transparent contracts to avoid disputes.
- Technology Adoption: Automate claims processing, eligibility checks, and payment reminders to reduce manual errors and delays.
- Data Analytics: Track metrics like DSO, denial rates, and net collection rates to identify bottlenecks. Use predictive tools for better decision-making.
- Outsourcing: For accounts over 90 days, outsourcing AR management can improve recovery rates and reduce administrative burdens.
Efficient AR processes minimize financial risks, improve collections, and support better cash flow management. Keep AR aging under control by combining automation, clear policies, and targeted follow-ups.
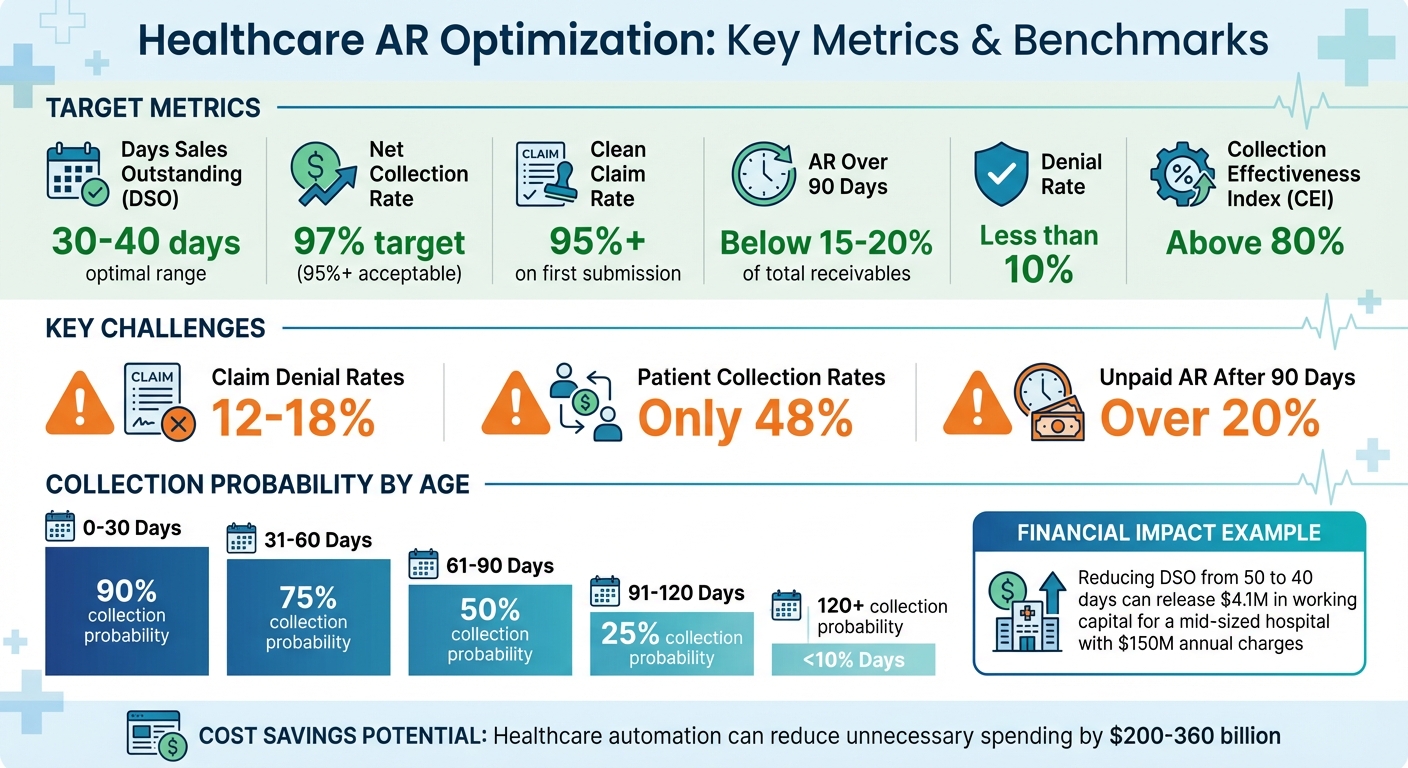
Healthcare AR Optimization: Key Metrics and Benchmarks
A Guide to Understanding Accounts Receivable (AR) | Medical Billers Network Live
Setting Up Clear Payment Policies and Communication
Managing accounts receivable (AR) effectively starts well before patients receive care. One essential step is implementing a written financial policy that patients sign during check-in. This document eliminates confusion by clearly outlining due dates, late fees, and patient responsibilities for co-pays and deductibles [8][5]. Margo Williams, MHA, CMPE, from the American College of Physicians, highlights the importance of accuracy in the process:
The most important function of the A/R process is to get that claim out right the first time [10].
Creating Transparent Payment Terms
A strong financial policy should state that co-pays and estimated deductibles are due at the time of service. Waiving co-pays is not an option, as insurers and federal law prohibit it [9][10]. As Robert L. Chiffelle, MHSA, explains:
The doctor's contract with the health plan provides for one fixed fee for each service... We cannot waive your portion of it; that is considered insurance fraud [9].
Another critical component is an "assignment of benefits" contract. This agreement allows your practice to bill and collect payments directly from the patient’s insurance. David Zetter, founder of Zetter Healthcare, cautions:
If an auditor sees that an assignment of benefits is worded incorrectly, and truly doesn't provide them the right to bill, then the payer can ask for every single dime back [10].
Additionally, be upfront about late fees - whether it’s a 1.5% monthly charge or a flat fee between $10 and $25 - and list all accepted payment methods, such as cash, credit cards, HSA/FSA, and online portals [8]. Clear payment terms ensure patients understand their financial obligations, setting the foundation for smoother transactions.
Teaching Patients About Insurance Coverage
Insurance confusion often leads to payment delays [11]. To avoid this, provide cost estimates before care, especially for elective or high-cost procedures. For example, deductibles for HSA-qualified plans can climb to $7,050 annually, while ACA-compliant plans may go as high as $8,700 [9]. Given these costs, it’s no surprise that over 50% of healthcare organizations now aim to collect 100% of a patient's financial responsibility before providing services [12]. This approach makes sense: the chances of collecting a balance drop to just 50% once it’s 61–90 days overdue [8].
Train your front-desk staff to use confident, polite language when discussing payments. Instead of asking, "Would you like to pay today?", say, "How would you like to take care of your balance today?" [8][9]. For larger balances, offer structured payment plans - for instance, collecting 50% upfront and spreading the rest over six months, or for balances over $600, requiring one-third upfront and the remainder over nine months [9]. Early payment incentives, such as a 2% discount for payments made within 10 days, can also encourage timely settlements [4]. Educating patients about their coverage and payment options reduces delays and helps lower Days Sales Outstanding (DSO).
Using Technology for Patient Communication
Digital tools can significantly improve payment response rates. Transitioning from paper statements to automated text messages and emails makes it easier for patients to stay informed and pay on time [11][4]. Features like automated reminders and patient portals provide instant access to balances, payment options, and installment plans [8][11][14]. Today, 90% of healthcare financial executives report having a patient portal in place [12].
Sending direct payment links via text or email further simplifies the process, allowing patients to resolve balances quickly on their mobile devices [11]. Integration is key: real-time synchronization between payment tools and your Practice Management or EHR systems ensures that balances update instantly, reducing manual errors and speeding up AR turnover [11][14]. By leveraging these technologies, practices can streamline communication, improve cash flow, and enhance the overall patient experience.
Improving AR Processes with Technology
Streamlining accounts receivable (AR) processes with the right technology can significantly reduce revenue cycle bottlenecks. By embracing automation and analytics, healthcare organizations stand to cut $200 billion to $360 billion in unnecessary spending [16]. The key? Shifting from reactive problem-solving to proactive error prevention.
Automating Claims Submission and Tracking
Automation tools can transform claims management, starting with claim scrubbers. These tools catch coding errors, missing modifiers, and mismatched diagnosis-procedure codes, helping organizations achieve a first-pass acceptance rate of 95% or higher [6][1]. Real-time eligibility verification ensures patients have active insurance, minimizing front-end errors [1][2]. For those initially categorized as self-pay, automated insurance discovery tools can uncover billable coverage - including retroactive Medicaid - for over 30% of cases [2]. One study revealed these tools could identify $50,000 in additional self-pay revenue per 1,000 claims by finding hidden coverage [2].
AI-driven medical coding takes automation a step further by performing real-time ICD-10 and CPT coding while ensuring compliance with payer-specific rules. It also flags undercoded services that might otherwise result in lost revenue [1]. After claims are submitted, automated status checks connect directly to payer portals, providing real-time updates without the need for manual follow-ups [2]. Additionally, Electronic Remittance Advice (ERA) tools automatically reconcile insurance payments with claims and bank deposits, saving time and reducing errors [6].
Christa Lassen-Vogel, Senior Manager at ZOLL Data Systems, highlights the importance of timely action:
The older the AR, the more difficult it is to collect within timely filing and timely appeals deadlines [2].
With claims submission optimized, the focus shifts to automating subsequent AR tasks.
Implementing AR Workflow Automation
Automation isn't limited to claims - it can enhance the entire AR lifecycle. Automated demographic verification ensures accurate patient data is available in seconds, improving data quality for 82% or more of patient encounters [2]. Deductible monitoring tools track when patients meet their deductibles, helping shift payment responsibilities efficiently [2]. Automated follow-up reminders standardize outreach efforts, ensuring unpaid claims are addressed every 15–30 days and denied claims within 5 days - without adding to administrative workloads [6][14].
Top-performing healthcare organizations aim to keep their Days in AR between 30 and 40 days [1][3]. For example, a mid-sized hospital with $150 million in annual charges could free up approximately $4.1 million in working capital by reducing AR from 50 to 40 days [1]. Integrating these tools with existing ERP or accounting platforms, such as QuickBooks, Oracle NetSuite, or Sage Intacct, ensures seamless data sharing between clinical and financial systems, creating a unified source of truth [14][17].
Alexandre, Finance Director at Upflow, sums it up well:
Revenue is only real when it turns into cash [14].
Managing Outstanding Balances
Once automation is in place, the next focus should be on collecting outstanding balances. The numbers don’t lie - collection probability drops dramatically from 90% within the first 30 days to less than 10% after 120 days [8]. Efficiently managing these balances is essential for maintaining a steady cash flow.
Segmenting Accounts by Risk and Payer Type
Breaking down accounts receivable (AR) by age, payer type, and balance size helps prioritize recoveries with the highest impact. Standard aging categories - 30, 60, 90, and over 120 days - offer a clear structure for escalation. Industry standards recommend keeping AR over 90 days below 15% to 20% of total receivables [6][2].
The type of payer is just as important as the age of the balance. Sorting receivables by insurance type (Medicare, major commercial insurers, or smaller payers) versus patient responsibility (self-pay, co-pays, deductibles) helps identify whether delays are due to payer processing issues or challenges in collecting from patients [8].
Prioritizing based on risk is key, especially for claims approaching timely filing or appeal deadlines. Missing these deadlines means losing any chance of recovery [18]. Christa Lassen-Vogel, Senior Manager at ZOLL Data Systems, highlights the urgency:
The older the AR, the more difficult it is to collect within timely filing and timely appeals deadlines [2].
High-dollar claims in the 90–120 day range often yield the best returns, making them top priorities [18][19].
| AR Aging Bucket | Likelihood of Collection | Priority Level |
|---|---|---|
| 0-30 Days | 90% | Low (Standard Billing) |
| 31-60 Days | 75% | Medium (Reminders) |
| 61-90 Days | 50% | High (Direct Contact) |
| 91-120 Days | 25% | Critical (Escalation) |
| 120+ Days | <10% | Last Resort (Collections/Write-off) |
Once high-priority accounts are identified, strict follow-up procedures can help reduce delays.
Creating Follow-Up Protocols
Strong follow-up systems ensure no accounts slip through the cracks. Best practices suggest contacting patients about unpaid claims every 15 to 30 days, while denied claims should be addressed within five days of notification [6]. A 2022 MGMA poll revealed that 42% of medical groups wait 91 to 120 days before sending accounts to collections, and 32% wait over 120 days - far too long given the sharp drop in collection likelihood [9].
Using multiple communication channels - phone, text, and email - can improve response rates [4]. When making calls, staff should identify the office, verify patient details, explain the insurance-paid amount, and request immediate payment via credit card or check [9]. Robert L. Chiffelle, MHSA, Principal with HSC Management, advises:
Using a collection agency is not a financially viable alternative except in the most extreme circumstances [9].
Collection agencies typically recover only 10% to 20% of balances and take 30% to 50% of the recovered amount as fees [9][8].
Training staff to use assertive yet professional language can also make a difference. Instead of asking, "Would you like to pay today?" encourage them to say, "How would you like to take care of your balance today?" [8]. Limit follow-up calls to three attempts before escalating the account [9]. Some practices introduce late fees, such as 1.5% per month or a flat $10 to $25, as long as this is clearly outlined in the financial policy [8].
Offering Flexible Payment Options
Flexible payment options can address common collection challenges and improve cash flow. Collecting co-pays and estimated deductibles at the time of registration reduces the need for back-end efforts [8]. For larger balances, structured payment plans are effective - for instance, requiring 50% upfront and spreading the rest over six months, or one-third upfront for balances over $600 [9].
Digital payment options significantly increase payment rates, with a 30% higher likelihood of success [20]. Provide options like credit cards, PayPal, mobile wallets, and online patient portals that offer 24/7 access [4]. Pre-authorized agreements, where a credit card is kept on file with patient consent, allow automatic billing once insurance processes the claim, eliminating excuses like "I forgot to pay" [8].
Early payment incentives are another strategy. One common model is the "2/10, net 30" discount, where patients get 2% off if they pay within 10 days instead of 30 [21][4]. Additionally, reminding patients about Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) can unlock funds they may have overlooked [8].
These flexible strategies reduce Days Sales Outstanding (DSO), lighten administrative workloads, and lower the risk of bad debt - keeping more revenue within the practice rather than losing 30-50% to collection agencies.
sbb-itb-e766981
Using Data Analytics to Optimize AR
Using data to make smarter decisions can significantly reduce claim denials - by as much as 20% - and shrink Days Sales Outstanding (DSO) by up to 60% [26][27]. Once you’ve streamlined processes with automation, diving into data analytics is the logical next step to fine-tune Accounts Receivable (AR) management.
Tracking Key AR Metrics
Focusing on the right metrics can reveal where revenue is stuck and how efficiently it’s moving. For example, Days Sales Outstanding (DSO) measures how quickly cash is recovered. In healthcare, a DSO under 30 days is considered strong, while 30–45 days is still acceptable [2][24].
Another key metric, the Net Collection Rate, shows the percentage of allowed reimbursement that’s actually collected. A target of 97% is ideal, but anything below 95% may point to inefficiencies. Amy Raymond, SVP of Revenue Cycle Operations and Deployments at AKASA, cautions:
Days in A/R can't be looked at in a vacuum. If your metrics are too good, it may not be the whole story. For example, you may be taking write-offs too quickly, which can skew the numbers in a positive direction [24].
Other important metrics include the denial rate (aim for less than 10%), the bad debt rate (the percentage of revenue written off as uncollectible), and the Collection Effectiveness Index (CEI), which evaluates the quality of collections. A CEI above 80% signals strong performance [22][25].
| Metric | Healthcare Benchmark | What It Reveals |
|---|---|---|
| Net Days in AR (DSO) | < 30 Days | Speed of cash recovery |
| Net Collection Rate | 97% | Success in collecting allowed amounts |
| AR Over 90 Days | < 20% | Volume of high-risk, aging revenue |
| Denial Rate | < 10% | Front-end or coding inefficiencies |
| CEI | > 80% | Quality of the collection process |
Tracking First Pass Claims Payment (FPCP) - the percentage of claims paid at 100% of the expected rate on the first try - can pinpoint front-end issues like coding or registration errors [24]. Amy Raymond emphasizes:
If health systems had to focus on one area to improve A/R days, it would be making sure everything is accurate before a claim goes out the door [24].
Using Predictive Analytics for Decision-Making
Building on automated workflows, predictive analytics takes decision-making to the next level by highlighting areas that need intervention. Instead of just analyzing past data, predictive tools forecast what’s likely to happen next. For example, they can estimate whether a claim will be accepted or rejected before it’s even submitted [28]. This allows teams to proactively address potential issues instead of reacting to denials.
Predictive models also help prioritize high-risk accounts, so staff can focus their efforts where they’ll have the most financial impact [28][29]. This approach, often referred to as “Receivable Intelligence,” makes it easier to allocate resources effectively [27][29].
These tools also improve cash flow forecasting by combining historical collection trends with expected cash sales, making it easier to manage working capital [22]. In fact, predictive analytics can boost revenue capture by 15% [26].
Here’s an example: A health system used an advanced AI platform to reduce A/R days by 13%. The platform leveraged machine learning to identify patterns in denials, leading to more effective claim follow-ups [24].
Another powerful use of analytics is tracking payer behavior. By monitoring denial rates and payment speeds for specific insurance carriers, teams can identify which payers frequently delay or deny claims. This insight can inform better negotiation strategies and help staff anticipate issues before they arise [28].
Conducting Regular AR Audits
While forecasting is essential, regular audits ensure everything stays on track. Audits catch errors before they turn into costly problems. Weekly AR report reviews can uncover trends and pending claims [6], while monthly process audits verify compliance with standard procedures [30][18].
Breaking down aging reports by categories like days (30, 60, 90, 120+), payer source, and denial reasons can expose systemic issues. For instance, if a specific payer repeatedly denies claims for the same reason, it’s a red flag that requires attention [18]. Audits should also include zero-balance reviews to spot underpayments and recover lost revenue [18][23]. Jesse Ford, President and CEO of Salud Revenue Partners, explains:
When claims close, an opportunity opens to increase payment accuracy and revenue [23].
For example, Salud Revenue Partners conducted a zero-balance review for a 10-hospital health system and uncovered $43 million in underpayments. Through targeted appeals, they recovered $21 million for the organization. In another case, an independent urban safety net hospital partnered with Salud Revenue Partners during March 2020. By leveraging data science and boutique recovery services, the hospital achieved a 22% drop in AR and a 56% reduction in bad debt [23].
Audits should also ensure compliance with CMS and federal regulations (Title 42 CFR). Pre-submission audits, using claim scrubbers or checklists, can catch errors early, aiming for a first-pass claim acceptance rate of 95% or higher [6][1]. Sharing audit results with clinical teams can improve documentation and coding accuracy, creating a feedback loop that helps prevent future denials [30].
When to Outsource AR Management
After establishing efficient internal workflows and leveraging data analytics, some healthcare organizations may find that outsourcing accounts receivable (AR) management is a practical next step. This isn't about admitting failure - it's about recognizing when specialized expertise can outperform in-house efforts.
Evaluating the Benefits of Outsourcing
A strong indicator that outsourcing might be the right move is when Days in A/R exceed 35, or when accounts older than 90 days make up more than 10%–22% of total receivables [31][32]. These benchmarks signal that revenue is lingering in the system for too long. Ryan Downs, Founding Partner at Real Partners Consulting, explains:
In nearly every circumstance, there is a dollar amount at which the costs associated with collecting a balance begin to exceed the amount of money collected. [7]
To make this calculation, you need to factor in salaries, benefits, technology costs, and overhead. If these expenses surpass the amount you're recovering, it's a clear sign your in-house process may be costing you more than it's worth [7].
When accounts pass the 120-day mark, collection rates drop significantly, making it even harder to justify the expense of in-house collections [32]. Outsourcing firms bring specialized knowledge in payer requirements and medical coding, which often leads to higher recovery rates and fewer claim denials. They also offer flexibility to scale services up or down based on patient volume - eliminating the need to hire or train additional staff [32][33].
Some organizations are turning to partial outsourcing, where only specific AR segments - like accounts over 90 days or workers' compensation claims - are sent to third-party providers. Newer accounts are kept in-house [34]. For example, HealthBridgeMD reports that its clients typically see a 30–45% reduction in AR days within 90 days of implementing outsourcing solutions [33].
Once you’ve determined that outsourcing is necessary, the next step is finding the right partner.
Choosing the Right AR Service Provider
The first thing to assess is the provider’s healthcare-specific expertise. It’s essential to choose a partner with a proven track record in hospital accounts receivable and a deep understanding of regional payer behaviors. General collections experience alone isn’t enough [32]. Ask for performance data that shows how they’ve improved collections compared to baseline metrics and verify their compliance with HIPAA, Medicare, and Medicaid [32].
Technology integration is another critical factor. Any provider you work with must integrate seamlessly with your existing Electronic Health Record (EHR) and billing systems to avoid creating data silos [32][33]. Look for providers that use AI-powered tools for tasks like claim scrubbing and denial tracking. These tools can save you from making costly investments in additional in-house software [34][35].
Before finalizing a partnership, establish clear Service Level Agreements (SLAs) tied to measurable outcomes such as cash-to-net ratio, denial rates, and AR days [32]. It’s also a good idea to have the provider review your AR data to create a pricing model that fits your budget [32]. Lastly, pay close attention to their communication protocols. A good partner will maintain your brand’s reputation and ensure positive interactions with patients throughout the collection process [15][32].
| AR Partnership Option | Responsibility | Ownership | Risk Level |
|---|---|---|---|
| Outsourcing | Partner | Provider | Shared/Provider |
| Factoring (with recourse) | Partner | Partner | Shared/Provider |
| Factoring (without recourse) | Partner | Partner | Partner |
| Financing | Provider | Provider | Provider |
Source: Real Partners Consulting / HFMA [7]
Shifting AR management to an outsourcing partner builds on prior process improvements, helping organizations optimize their revenue cycle further.
Conclusion
Improving AR in healthcare relies on clear policies, advanced tools, proactive strategies, and actionable insights. Automating tasks like claim scrubbing and payment reminders not only streamlines operations but also allows your team to focus more on patient care rather than chasing overdue payments [13][1][30].
These changes can lead to noticeable financial gains. For instance, cutting AR by just 10 days can unlock substantial working capital [1]. Top-performing organizations aim for Days in AR between 30 and 40 days and maintain clean claim rates above 95% [3][6]. These benchmarks aren't random - they highlight the difference between a healthy cash flow that drives growth and funds stuck in aging receivables.
Speed matters when it comes to collections. The odds of recovering a patient balance plummet from 90% within the first 30 days to under 10% after 120 days [8]. That’s why segmenting AR by aging buckets and focusing on high-value claims is crucial. Reviewing AR aging reports weekly ensures problems are addressed before they escalate [8][6].
Technology also plays a key role in sustaining these improvements. Use real-time dashboards to monitor essential metrics like net collection ratio (target: 96%+), denial rates, and AR aging. This data helps pinpoint bottlenecks and enables quick, informed decisions [6][1]. If internal efforts stall or Days in AR consistently exceed 45–50 days, outsourcing older accounts - such as those over 90 days - can bring specialized expertise and improve recovery rates [6][1].
FAQs
How can healthcare companies lower their Days Sales Outstanding (DSO)?
Days Sales Outstanding (DSO) tracks how long it takes a healthcare organization to collect payments after providing services. When DSO is too high, it can disrupt cash flow, increase expenses, and limit the ability to invest in areas like patient care or new technologies. Ideally, DSO should remain below 45 days to maintain financial health.
To keep DSO in check, healthcare organizations can refine their revenue cycle processes. One key step is verifying insurance eligibility and collecting copays or deductibles upfront, which helps avoid payment delays. Automating claims submission and integrating tools like AI for collections can streamline payment posting and quickly flag overdue accounts for follow-up. Promptly addressing rejected claims also ensures revenue doesn’t get stuck in limbo.
Offering patients flexible payment options - such as online portals or installment plans - and providing clear, itemized billing statements can further speed up collections. Regular follow-ups on unpaid invoices, supported by automated reminders, can prevent balances from aging beyond 90 days. By adopting these practices, healthcare providers can maintain a DSO in the 30–45 day range, ensuring steady cash flow and greater operational flexibility.
How does technology improve accounts receivable (AR) processes in healthcare?
Technology is reshaping healthcare accounts receivable (AR) processes, making operations smoother and boosting cash flow. By automating repetitive tasks like claim submissions, eligibility checks, and payment postings, healthcare providers can cut down on manual mistakes, speed up collections, and reduce days sales outstanding (DSO). Tools powered by AI and analytics also allow providers to spot denial patterns, underpayments, and coding issues in real time, paving the way for quicker solutions and stronger financial performance.
Modern tools, including AI-driven collection systems, robotic process automation (RPA) for validating claims, and cloud-based AR platforms, integrate effortlessly with electronic health record (EHR) and billing systems. These technologies simplify billing, expand digital payment options, and streamline dispute resolution processes. The result? Greater operational efficiency and improved patient satisfaction. For healthcare providers looking to adopt these solutions, Phoenix Strategy Group offers guidance in choosing and implementing the right tools to align AR processes with financial objectives and achieve better outcomes.
When should healthcare organizations outsource accounts receivable (AR) management?
Healthcare organizations may want to think about outsourcing their accounts receivable (AR) management when internal teams face challenges like maintaining cash flow or handling increasing administrative tasks. Some clear red flags include AR aging past 90 days, as the chances of collection drop sharply after that point, or a Days Sales Outstanding (DSO) that consistently exceeds industry standards, which points to delayed payments and tied-up capital. Other indicators include frequent claim denials, navigating complicated payer rules, and ongoing staffing shortages.
By outsourcing AR, healthcare providers can speed up payment cycles, cut down on administrative expenses, and enhance compliance. Partnering with a company like Phoenix Strategy Group offers access to specialized expertise, advanced tools, and customized financial strategies. This allows healthcare organizations to streamline AR processes, lower DSO, and give their internal teams more time to focus on providing excellent patient care.